Should You Get All Your Vaccines in the Same Arm?, Successful Transplant of an Engineered Pig Kidney, Updated Practice Guidelines for Postdural Headache, Deep Brain Stimulation Improves Upper Limb Paralysis Post-Stroke.
The Full Panel meets your TLDR (Too Long; Didn’t Read) needs by delivering the latest medicine & health news in a nutshell. 🥜
Should you get all your COVID shots in the same arm? 💉

Gist: A recent study suggests that getting both doses of a sequential vaccine, like the Pfizer-BioNTech COVID-19 vaccine, in the same arm might boost the body's immune response. This approach, known as "ipsilateral vaccination", was compared with "contralateral vaccination", where the first and second doses are given in opposite arms.
Nitty-Gritty: German researchers analyzed the data of 303 individuals who took the Pfizer-BioNTech vaccine. They specifically compared the immune responses of 147 people who received both doses in the same arm to 156 people who got their shots in different arms. An additional focus was placed on a subgroup of 143 participants, examining their specific immune cells.
Results revealed that while the overall antibody levels were similar between the two groups, those who were vaccinated in the same arm showed stronger neutralizing activity against the virus. Moreover, 67% of these individuals had detectable killer T cells, compared to only 43% in the group vaccinated in opposite arms.
Big Picture: Laura Ziegler from Saarland University emphasized that the study found ipsilateral vaccinations produce a more robust immune response. Although the findings are promising, further research is needed. One theory for the improved response is that the same lymph nodes are used for both vaccine doses, optimizing the body's defense mechanism.
Original source: here.
Surgeons at NYU Langone Health successfully transplanted a genetically engineered pig kidney

Gist: Surgeons at NYU Langone Health successfully transplanted a genetically engineered pig kidney into a deceased human, marking the longest period (32 days) a gene-edited pig kidney has functioned in a human. This monumental procedure, held on July 14, 2023, under Dr. Robert Montgomery, is the fifth xenotransplant performed at NYU Langone and represents significant progress towards a sustainable organ transplant supply.
Nitty-Gritty: Dr. Montgomery emphasized that the pig kidney, with just one genetic modification, effectively replaced a human kidney's function for over 32 days without rejection. The primary challenge with xenotransplants is preventing hyperacute rejection. To counter this, scientists "knocked out" the gene responsible for rapid antibody-mediated rejection of pig organs in humans. Moreover, the pig's thymus gland was embedded in the kidney to deter new immune responses, thus ensuring organ acceptance. The thymus is the organ primarily responsible for the production and maturation of immune cells.
The study showed that removing the patient's native kidneys and replacing them with one pig kidney resulted in optimal kidney function. Creatinine levels, indicative of kidney function, remained in the desired range, and there was no biopsy evidence of rejection.
Big Picture: In the U.S., over 103,000 people await a transplant, with around 88,000 in line for a kidney. Dr. Montgomery believes xenotransplantation can address this organ scarcity. The pig kidney was sourced from a GalSafeTM pig, approved by the FDA in 2020. Interestingly, despite previous experiments using up to 10 genetic modifications, this study revealed that a single modification might suffice.
The research, facilitated by the donation of a 57-year-old male's body post-brain death and collaboration with LiveOnNY, suggests we are nearing clinical trials. Dr. Montgomery anticipates this could potentially save thousands of lives, emphasizing the need for safety and care in advancing this procedure.
Original source: here.
New practice guidelines for postdural puncture headache 🧠
Gist: New guidelines have been released to address postdural puncture headaches (PDPH), a known complication arising from certain medical procedures involving the spinal area. The guidelines were recently developed by the American Society for Regional Anesthesia and Pain Medicine, in association with five other major medical organizations. Published in the JAMA Network Open, these guidelines offer structured recommendations on risk factors, diagnosis, preventive measures, and treatment options related to PDPH.
Nitty-Gritty: PDPH is a type of headache that can be so severe that it keeps patients bedridden. It can be especially challenging for new mothers recovering from childbirth. The likelihood of developing PDPH after a procedure can range anywhere from 2% to 40%, depending on the procedure and individual patient factors.
While numerous reviews have discussed PDPH, consistent and evidence-backed recommendations have been lacking. These new guidelines offer 37 statements and 47 specific recommendations, which have achieved a near-unanimous consensus among experts. They highlight the importance of understanding the risks before any procedure and recommend that healthcare centers have robust post-procedure follow-up policies for patients.
Big Picture: Although these guidelines mark a significant step forward, they also underscore the need for further research in the field. Nevertheless, they provide a much-needed framework to help healthcare professionals better diagnose, assess risk, and manage PDPH.
Original source: here.
Deep brain stimulation may enhance upper limb function post-stroke
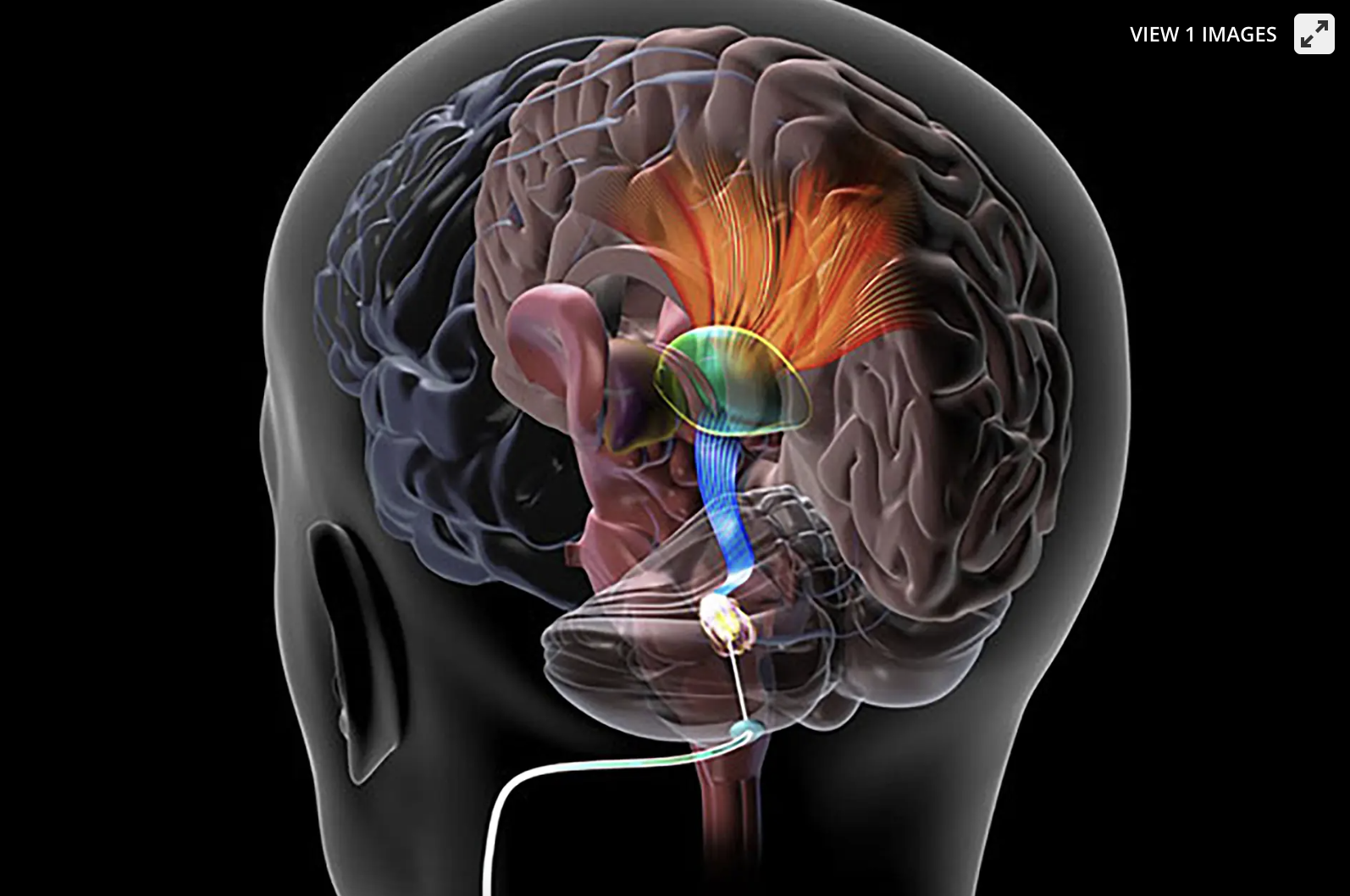
Gist: In an early-phase clinical trial, researchers observed that deep brain stimulation (DBS) of the cerebellum may assist in the recovery of upper limb function following a stroke. The study involved 12 participants with significant upper extremity impairment post-stroke. When combined with rehabilitation, DBS to the cerebellum's dentate nucleus (DN) resulted in 75% of these participants regaining some functionality in their paralyzed arms. Additionally, PET scans showcased notable increments in brain metabolism around the stroke-affected region.
Nitty-Gritty: The study's authors state that these results demonstrate the safety and feasibility of using DBS in the cerebellar dentate nucleus to promote neuroplasticity and functional recovery. André Machado, MD, PhD, of the Cleveland Clinic, emphasized the promise of the Phase I study results but indicated that further research is required, with a Phase II clinical trial already in progress.
Neuroplasticity, the brain's ability to reorganize itself, plays a pivotal role in post-stroke recovery. The research introduces a novel surgical method aimed at extending neuroplasticity after ischemic and traumatic brain events. This involves stimulating the cerebellar DN to activate neural pathways, promoting cerebral cortex reorganization around stroke-affected areas and boosting cortical activity.
Big Picture: The trial revealed that participants maintained their treatment-related improvements, with no significant adverse events recorded. National and international experts have lauded the study, advocating for larger controlled trials to validate the results.
Original source: here.
Interested in previous newsletters or other articles we’ve published? Check them out here at: thefullpanel.com
Got a question for us? Suggestions for content you’d like to see? Feedback? E-mail us at: hello@mail.thefullpanel.com
